Obesity surgery, also known as bariatric surgery, has emerged as a life-changing intervention for individuals battling severe obesity and its associated health conditions. This medical procedure is designed to help patients achieve significant and sustainable weight loss, improve their quality of life, and reduce the risk of obesity-related diseases. In this article, we explore the various types of obesity surgery, their benefits, risks, and the lifestyle changes necessary for long-term success.
Page Contents
Understanding Obesity Surgery
cirugia de obesidad encompasses a range of procedures aimed at reducing the stomach’s capacity or altering the digestive process to promote weight loss. These surgeries are typically recommended for individuals who:
- Have a Body Mass Index (BMI) of 40 or higher: This is categorized as severe obesity.
- Have a BMI of 35-39.9 with Obesity-Related Conditions: Such as type 2 diabetes, hypertension, sleep apnea, or joint problems.
- Have Not Achieved Success with Non-Surgical Methods: Including diet, exercise, and medication.
Candidates must undergo a thorough evaluation to determine their suitability for surgery, including medical tests, nutritional counseling, and psychological assessments.
Types of Obesity Surgery
There are several types of obesity surgery, each with unique mechanisms and benefits. The most common procedures include:
1. Sleeve Gastrectomy
- Procedure: Removes about 75-80% of the stomach, leaving a tube-shaped “sleeve.”
- Mechanism: Limits food intake and reduces hunger by decreasing the production of the hunger hormone ghrelin.
- Benefits: Significant weight loss and improvement in metabolic conditions.
2. Gastric Bypass (Roux-en-Y)
- Procedure: Creates a small pouch from the stomach and connects it directly to the small intestine.
- Mechanism: Reduces calorie absorption and limits food intake.
- Benefits: Effective for long-term weight loss and resolving type 2 diabetes.
3. Adjustable Gastric Banding
- Procedure: Places an inflatable band around the upper part of the stomach to create a smaller stomach pouch.
- Mechanism: Restricts food intake by slowing digestion.
- Benefits: Adjustable and reversible, with fewer complications compared to other procedures.
4. Biliopancreatic Diversion with Duodenal Switch (BPD/DS)
- Procedure: Combines a sleeve gastrectomy with intestinal rerouting.
- Mechanism: Limits food intake and significantly reduces calorie absorption.
- Benefits: Most effective for weight loss but involves higher risks and nutritional deficiencies.
Benefits of Obesity Surgery
Obesity surgery offers numerous health and lifestyle benefits, including:
- Significant Weight Loss: Patients can lose 50-70% of their excess weight within 12-18 months.
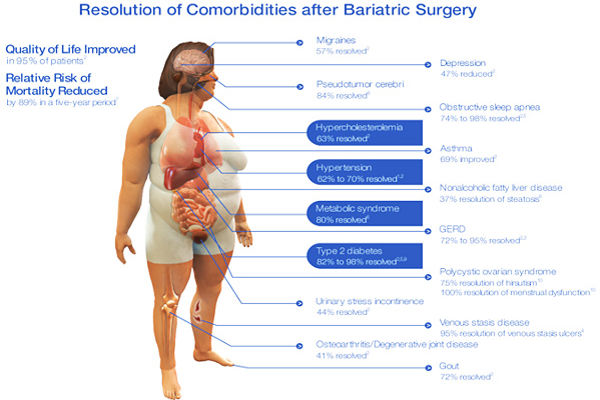
- Improved Health Conditions: Resolves or alleviates type 2 diabetes, high blood pressure, sleep apnea, and joint pain.
- Enhanced Mobility: Reduced weight makes physical activities easier and more enjoyable.
- Increased Longevity: Studies show that bariatric surgery can reduce the risk of premature death from obesity-related causes.
- Better Quality of Life: Many patients report improved self-esteem, energy levels, and mental health.
Risks and Complications
As with any surgery, obesity surgery carries potential risks and complications, including:
- Surgical Risks: Infection, bleeding, or adverse reactions to anesthesia.
- Nutritional Deficiencies: Reduced absorption of vitamins and minerals may require lifelong supplementation.
- Dumping Syndrome: Rapid gastric emptying can cause nausea, vomiting, and diarrhea.
- Gallstones: Rapid weight loss increases the risk of developing gallstones.
- Weight Regain: Without adherence to lifestyle changes, some patients may regain weight over time.
Life After Obesity Surgery
Success after obesity surgery depends on a commitment to lifelong lifestyle changes. Here’s what patients can expect:
Dietary Adjustments
- Follow a Progressive Diet: Transition from liquids to pureed, soft, and then solid foods over weeks.
- Smaller Portions: The reduced stomach size requires smaller, more frequent meals.
- High-Protein Diet: Protein supports muscle maintenance and overall health.
- Avoid Sugary and Fatty Foods: These can cause discomfort and hinder weight loss.
- Stay Hydrated: Drink water throughout the day but avoid drinking during meals.
Exercise Routine
Regular physical activity is crucial for maintaining weight loss and improving overall health. Patients are encouraged to:
- Start with light activities like walking.
- Gradually increase the intensity and duration of workouts.
- Incorporate strength training to build muscle and boost metabolism.
Psychological Support
Emotional and psychological support is vital for long-term success. Patients can benefit from:
- Counseling: To address emotional eating and adapt to lifestyle changes.
- Support Groups: Connecting with others who have undergone similar procedures for shared experiences and encouragement.
Regular Follow-Up Care
Post-surgery check-ups are essential to:
- Monitor weight loss and nutritional status.
- Address complications or concerns.
- Adjust dietary and exercise plans as needed.
Is Obesity Surgery Right for You?
Deciding to undergo obesity surgery is a personal decision that requires careful consideration and consultation with a qualified bariatric surgeon. It is important to weigh the benefits against the risks and to be prepared for the lifestyle changes necessary to achieve and maintain success.
Conclusion
Obesity surgery is a powerful tool for combating severe obesity and its associated health challenges. By reducing stomach size or altering digestion, these procedures help patients achieve significant weight loss, improve their health, and enhance their quality of life.
However, the journey doesn’t end with surgery—it requires a lifelong commitment to healthy eating, regular exercise, and ongoing medical care. If you’re considering obesity surgery, consult with your healthcare provider to explore your options and determine the best path forward.