Migraines can be incredibly debilitating, disrupting daily life with severe symptoms. Among the various types of migraines, basilar-type migraine stands out due to its unique and often more intense manifestations. Understanding these migraine symptoms and exploring effective relief strategies is crucial for managing this condition. Dr. Chandril Chugh, a leading neurologist, provides comprehensive insights into basilar-type migraine symptoms and offers practical strategies for finding relief.
Page Contents
What is Basilar-Type Migraine?
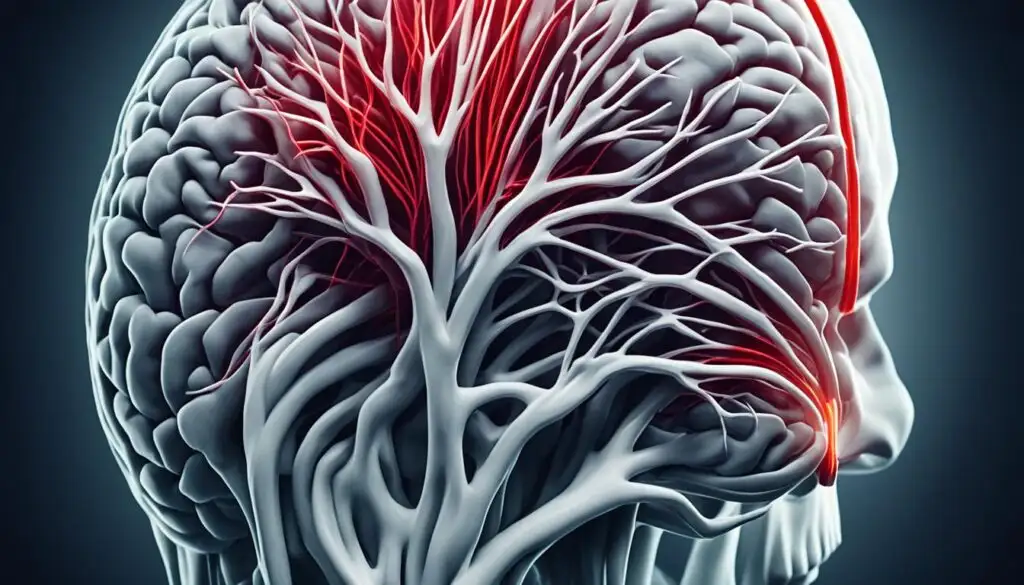
Basilar-type migraine, also known as basilar artery migraine, is a rare form of migraine that primarily affects the brainstem and posterior circulation of the brain. Unlike more common migraines, basilar-type migraines involve neurological symptoms related to the brainstem, leading to a distinctive and often more severe presentation.
Characteristics of Basilar-Type Migraine
- Neurological symptoms that precede the headache phase.
- Symptoms originating from the brainstem or both hemispheres of the brain.
- Affects vision, coordination, and balance.
- Common in adolescents and young adults, particularly females.
Recognizing Basilar-Type Migraine Symptoms
Understanding basilar migraine symptoms is crucial for timely diagnosis and management. These symptoms can be alarming and may mimic other neurological conditions, making accurate identification vital for effective treatment.
Aura Symptoms
Aura symptoms often precede the headache phase in basilar-type migraines. These neurological disturbances typically last between 5 to 60 minutes and can include:
- Visual Disturbances: Seeing flashes of light, blind spots, or zigzag patterns. Patients may experience double vision or temporary loss of vision in one or both eyes.
- Vertigo: A sensation of spinning or dizziness can occur, affecting balance and coordination. Vertigo in basilar migraines may be intense and disorienting.
- Speech Difficulties: Some individuals may struggle with speech, experiencing slurred speech or difficulty finding words.
- Tinnitus: Ringing in the ears or hearing unusual sounds can be a symptom of basilar-type migraine.
- Numbness and Tingling: Patients may feel numbness or tingling in the face, arms, or legs, often on one side of the body.
Headache Phase
Following the aura, the headache phase of a basilar migraine typically begins. The headache is usually throbbing or pulsating and can be severe. It often starts at the back of the head and may radiate to the front. This phase can last from several hours to a few days and may include:
- Intense Throbbing Pain: The headache is often described as severe and incapacitating, affecting the ability to perform daily activities.
- Nausea and Vomiting: Nausea and vomiting frequently accompany the headache, worsening the overall discomfort.
- Sensitivity to Light and Sound: Patients may become highly sensitive to light (photophobia) and sound (phonophobia), necessitating a dark and quiet environment.
Postdrome Phase
After the headache subsides, many individuals experience a postdrome phase, often referred to as a “migraine hangover.” Symptoms during this phase can include:
- Fatigue: Extreme tiredness and a feeling of being drained are common.
- Difficulty Concentrating: Patients may struggle with concentration and cognitive function.
- Mood Changes: Feelings of irritability or depression can occur as the body recovers from the migraine.
Causes and Triggers of Basilar-Type Migraine
The exact cause of basilar-type migraine remains unclear. However, several factors may contribute to its development. Identifying and avoiding triggers can help manage the frequency and severity of attacks.
Genetic Factors
Genetics may play a role in basilar-type migraines, as a family history of migraines increases the likelihood of experiencing this condition. Understanding your family medical history can provide valuable insights into potential genetic links.
Hormonal Changes
Hormonal fluctuations, particularly in females, can trigger basilar-type migraines. Changes related to the menstrual cycle, pregnancy, or menopause can influence migraine patterns.
Environmental Triggers
Environmental factors, such as exposure to bright lights, loud noises, or strong odors, can precipitate basilar migraine symptoms. Stress, lack of sleep, and changes in weather are also common triggers.
Dietary Factors
Certain foods and beverages may trigger basilar-type migraines in susceptible individuals. Common dietary triggers include:
- Caffeine: Excessive caffeine consumption or withdrawal can trigger migraines.
- Alcohol: Particularly red wine and other alcoholic beverages can precipitate attacks.
- Processed Foods: Foods containing additives, preservatives, or artificial sweeteners may trigger symptoms.
- Aged Cheeses and Cured Meats: These foods often contain tyramine, a substance known to provoke migraines.
Diagnosing Basilar-Type Migraine
Accurate diagnosis of basilar-type migraine is essential for effective management. Dr. Chandril Chugh outlines the diagnostic process to differentiate basilar migraine from other conditions with similar symptoms.
Comprehensive Medical History
Gathering a detailed medical history helps identify patterns and triggers associated with basilar-type migraine. Information about family history, frequency of attacks, and specific symptoms provides valuable diagnostic clues.
Neurological Examination
A thorough neurological examination assesses motor function, coordination, and sensory responses. This examination helps identify any abnormalities and rule out other potential causes of symptoms.
Imaging Studies
In some cases, imaging studies such as MRI or CT scans may be necessary to exclude other neurological conditions that can mimic basilar-type migraine. These studies provide detailed images of the brain and its structures.
Evaluation of Aura Symptoms
Evaluating the nature and progression of aura symptoms is crucial for diagnosing basilar-type migraine. Aura symptoms that involve both visual and non-visual disturbances, particularly those originating from the brainstem, are indicative of this migraine type.
Relief Strategies for Basilar-Type Migraine
Managing basilar migraine symptoms involves a combination of lifestyle modifications, preventive measures, and acute treatments. Dr. Chandril Chugh shares effective relief strategies to help patients manage their condition and reduce the frequency of attacks.
Lifestyle Modifications
Adopting healthy lifestyle habits can significantly impact the management of basilar-type migraines. Key lifestyle modifications include:
- Stress Management: Implementing stress reduction techniques such as meditation, yoga, or deep breathing exercises can help prevent migraines triggered by stress.
- Regular Sleep Schedule: Maintaining a consistent sleep schedule and ensuring adequate rest are crucial for preventing migraines.
- Healthy Diet: Avoiding dietary triggers and maintaining a balanced diet rich in fruits, vegetables, and whole grains supports overall health and reduces migraine risk.
- Hydration: Staying well-hydrated is essential for minimizing the likelihood of dehydration-induced migraines.
Preventive Medications
Preventive medications can reduce the frequency and severity of basilar-type migraines. These medications are typically taken daily and may include:
- Beta-Blockers: Medications like propranolol help prevent migraines by regulating blood flow and reducing the frequency of attacks.
- Calcium Channel Blockers: Verapamil is often used to prevent migraines by stabilizing blood vessel constriction.
- Antidepressants: Tricyclic antidepressants or selective serotonin reuptake inhibitors (SSRIs) can be effective in preventing migraines.
- Antiepileptic Drugs: Medications such as topiramate or valproate help stabilize brain activity and prevent migraine onset.
Acute Treatments
Acute treatments focus on relieving symptoms during a migraine attack. Dr. Chandril Chugh recommends several options for managing acute migraine symptoms:
- Triptans: Triptans, such as sumatriptan, are commonly used to treat migraines. They work by narrowing blood vessels and blocking pain pathways in the brain.
- NSAIDs: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or aspirin can help alleviate pain and inflammation associated with migraines.
- Anti-Nausea Medications: Medications like metoclopramide can relieve nausea and vomiting often accompanying migraines.
- Ergotamines: Ergotamine derivatives, such as dihydroergotamine, can be effective in treating migraines but are used less frequently due to side effects.
Non-Pharmacological Therapies
Non-pharmacological therapies can complement medical treatments and provide additional relief. These therapies include:
- Cognitive Behavioral Therapy (CBT): CBT helps patients manage stress, anxiety, and other emotional factors that may trigger migraines.
- Biofeedback: Biofeedback techniques teach patients to control physiological responses, such as muscle tension and heart rate, to prevent migraines.
- Acupuncture: Acupuncture involves inserting thin needles into specific points on the body to alleviate pain and reduce migraine frequency.
Coping Strategies for Basilar-Type Migraine
Living with basilar-type migraine requires effective coping strategies to manage symptoms and maintain quality of life. Dr. Chandril Chugh offers practical advice for coping with this challenging condition.
Create a Migraine-Friendly Environment
Designing a migraine-friendly environment can help minimize triggers and provide a comfortable space during an attack. Use soft lighting, reduce noise levels, and keep a quiet, dark room available for rest.
Maintain a Migraine Diary
Keeping a migraine diary helps track the frequency, duration, and triggers of migraine attacks. This information is valuable for identifying patterns and making informed decisions about treatment and lifestyle adjustments.
Educate Yourself and Others
Understanding basilar-type migraine and educating family, friends, and coworkers about the condition fosters a supportive environment. Awareness of symptoms and triggers can help others provide appropriate assistance and accommodations.
Plan for Emergencies
Having an emergency plan in place ensures preparedness for severe migraine attacks. Keep a supply of acute medications, contact information for healthcare providers, and a list of emergency contacts readily available.
Seek Support
Joining support groups or online communities for individuals with migraines provides a platform for sharing experiences, coping strategies, and emotional support. Connecting with others who understand the challenges of living with basilar-type migraine can be empowering.
Conclusion
Basilar-type migraine presents a unique set of challenges due to its distinctive symptoms and neurological impact. Dr. Chandril Chugh’s insights into basilar migraine symptoms and relief strategies offer valuable guidance for those affected by this rare condition. By understanding the symptoms, exploring treatment options, and implementing effective coping strategies, individuals with basilar-type migraine can manage their condition and improve their quality of life.
For more information on managing basilar migraine symptoms, visit basilar migraine symptoms. Embrace the journey of managing basilar-type migraine with confidence and take proactive steps toward better health and well-being.
Also Read:
The Effective Home Remedies for Constipation: A Comprehensive Guide
The Wonderful Benefits of Wheat Grass Powder: A Comprehensive Guide