Asthma, a chronic respiratory condition affecting millions worldwide, has traditionally been categorized as a disorder driven by allergic or environmental triggers. However, as the understanding of immunology evolves, researchers are exploring the intricate relationship between asthma and autoimmunity. In this article, we will delve into the current state of knowledge regarding the potential autoimmune aspects of asthma and the implications for diagnosis and treatment.
Page Contents
Asthma Overview
Asthma is characterized by inflammation of the airways, leading to symptoms such as wheezing, shortness of breath, chest tightness, and coughing. Common triggers include allergens like pollen, dust mites, and pet dander. Traditionally, asthma has been viewed as an allergic or hypersensitivity disorder, with the immune system responding excessively to these environmental factors.
Key Features of Asthma
Airway Inflammation
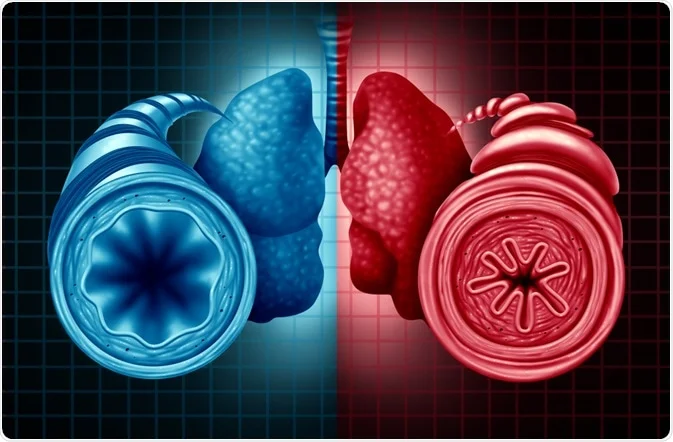
The inflammation of the airways is a hallmark feature of asthma. This inflammation makes the airways more susceptible to irritation and triggers, leading to the characteristic symptoms.
Bronchoconstriction
In response to triggers, the muscles around the airways may tighten (bronchoconstriction), further narrowing the passage for air to flow. This constriction contributes to the difficulty in breathing experienced by individuals with asthma.
Increased Mucus Production
Asthma can stimulate the production of excess mucus in the airways. This mucus further obstructs airflow, making it challenging for individuals with asthma to breathe freely.
Triggers and Contributing Factors
Allergens
Common allergens such as pollen, mold, pet dander, dust mites, and certain foods can trigger asthma symptoms.
Irritants
Environmental irritants, including tobacco smoke, air pollution, strong odors, and chemical fumes, can exacerbate asthma symptoms.
Respiratory Infections
Viral respiratory infections, such as the common cold or flu, can trigger asthma attacks.
Physical Activity
Exercise or physical exertion can induce asthma symptoms, known as exercise-induced bronchoconstriction.
Weather Changes
Cold air, changes in temperature, and humidity levels can impact individuals with asthma.
Occupational Exposures
Some individuals may experience asthma symptoms due to exposure to certain substances in the workplace.
Diagnosis
Asthma diagnosis typically involves a combination of medical history, physical examination, and lung function tests. Common diagnostic tools include spirometry, which measures the amount and speed of air breathed in and out, and peak flow measurements.
Treatment and Management
Bronchodilators
These medications relax the muscles around the airways, helping to alleviate bronchoconstriction and improve airflow.
Anti-Inflammatory Medications
Corticosteroids and other anti-inflammatory drugs are used to reduce airway inflammation and prevent asthma symptoms.
Long-Term Control Medications
For individuals with persistent asthma, long-term control medications, such as leukotriene modifiers or long-acting beta-agonists, may be prescribed.
Allergen Management
Identifying and managing exposure to allergens is crucial in asthma management. This may involve lifestyle modifications and, in some cases, immunotherapy.
Asthma and Autoimmunity Action Plan
Empowering individuals with asthma with knowledge about their asthma and autoimmunity personalized action plans help them manage symptoms effectively.
Monitoring and Regular Check-ups
Regular monitoring of asthma symptoms, peak flow measurements, and scheduled check-ups with healthcare providers are essential for maintaining asthma control.
Autoimmunity Defined
Autoimmunity occurs when the immune system mistakenly targets and attacks the body’s own tissues. In classic autoimmune diseases like rheumatoid arthritis or lupus, the immune system loses its ability to distinguish between self and non-self, leading to an attack on the body’s organs or tissues.
The Emerging Autoimmune Aspect of Asthma
While asthma has not been officially classified as an autoimmune disease, recent research has uncovered intriguing links between certain immunological features found in autoimmune conditions and asthma. These findings have prompted scientists to explore the potential autoimmune mechanisms at play in certain asthma subtypes.
Shared Immunological Features
Studies have identified shared immunological features between autoimmune asthma and autoimmunity. Both involve dysregulation of T-helper cells, cytokines, and other immune components. For example, elevated levels of certain autoantibodies have been found in the lungs of some individuals with asthma, indicating a potential autoimmune component.
Genetic Links
Genetics play a role in both autoimmune asthma and autoimmunity. Certain genetic factors associated with autoimmune conditions have been found to influence asthma susceptibility. This genetic overlap suggests shared underlying mechanisms that merit further investigation.
Key Points Regarding Genetic Links in Asthma
Familial Clustering
Asthma tends to run in families, suggesting a strong genetic predisposition. If a person has parents or siblings with asthma, their likelihood of developing asthma is increased.
Polygenic Inheritance
Asthma is considered a polygenic disorder, meaning that multiple genes contribute to its development. Various genes associated with immune responses, inflammation, and airway function play a role in asthma susceptibility.
Implications for Asthma Research and Treatment
Personalized Medicine
Understanding the genetic basis of asthma allows for a more personalized approach to treatment. Identifying specific genetic factors can help tailor interventions to target the underlying mechanisms contributing to asthma in individual patients.
Early Detection and Prevention
Genetic information may contribute to early detection and prevention strategies. Identifying individuals at a higher genetic risk could lead to targeted preventive measures, such as avoiding certain environmental triggers or implementing early interventions.
Drug Development
Insights into the genetic basis of asthma can inform drug development. Targeting specific pathways influenced by genetic factors may lead to the development of more effective and targeted medications.
Gene Therapy
While still in its early stages, research into gene therapy for asthma holds promise. Modifying or replacing specific genes associated with asthma susceptibility could potentially offer novel therapeutic approaches.
Environmental Triggers and Autoimmunity
Environmental factors known to trigger asthma, such as pollution and respiratory infections, have also been linked to the development or exacerbation of autoimmune diseases. This intersection raises intriguing possibilities regarding the complex interplay between environmental triggers, the immune system, and asthma.
Key Points Regarding Environmental Triggers and Autoimmunity
- Exposure to Chemicals and Toxins
- Certain environmental pollutants, chemicals, and toxins have been linked to an increased risk of autoimmune diseases. Prolonged exposure to substances such as heavy metals, solvents, and pesticides may contribute to the development of autoimmune conditions.
- Infections and Microbial Triggers:
- Infections, particularly chronic or persistent ones, can trigger or exacerbate autoimmune responses. Microorganisms, including asthma and autoimmunity can stimulate the immune system in a way that may lead to the misidentification of self-tissues as foreign.
- Hygiene Hypothesis:
- The hygiene hypothesis suggests that reduced exposure to infections and microbes in early childhood may contribute to an increased risk of autoimmune diseases. Lack of early immune system challenges may lead to dysregulation and the development of autoimmune responses.
Clinical Implications
Recognizing the potential autoimmune aspects of asthma has significant clinical implications. It opens new avenues for personalized treatment approaches that target specific immune pathways. Immunomodulatory therapies, commonly used in autoimmune conditions, could be explored as potential interventions for certain asthma subtypes.
Challenges and Questions
While the autoimmune connection in asthma is a fascinating area of research, challenges and unanswered questions remain. It’s essential to note that not all cases of asthma involve autoimmune mechanisms, and the relationship is likely complex and multifaceted. Further research is needed to identify specific subtypes of asthma where autoimmune processes play a significant role.
Conclusion
In conclusion, the evolving understanding of asthma’s immunological landscape introduces a new dimension to the traditional narrative. While asthma has long been viewed primarily through the lens of allergic responses, the potential autoimmune connection adds complexity to the picture. Unraveling the intricacies of asthma’s relationship with the immune system could pave the way for more targeted and effective therapies, offering hope for better management and improved quality of life for individuals living with asthma. As research progresses, the intersection of asthma and autoimmunity promises to reveal new insights, shaping the future of respiratory medicine.




